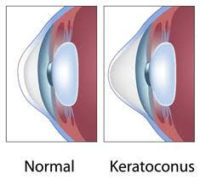
 Keratoconus is a progressive condition that occurs with thinning and distortion of the cornea. Doctors do not yet know what causes keratoconus, although in some cases it appears to be genetic. About 1 out of 10 people with keratoconus have a parent who has it, too. Keratoconus often starts when people are in their late teens the to early 20s. The vision symptoms slowly get worse over a period of about 10 to 20 years. This condition appears to equally affect both males and females and is present within all ethnicities. Keratoconus can be diagnosed through a routine eye exam. This condition generally involves both eyes, although one eye may be more affected than the other.
Keratoconus is a progressive condition that occurs with thinning and distortion of the cornea. Doctors do not yet know what causes keratoconus, although in some cases it appears to be genetic. About 1 out of 10 people with keratoconus have a parent who has it, too. Keratoconus often starts when people are in their late teens the to early 20s. The vision symptoms slowly get worse over a period of about 10 to 20 years. This condition appears to equally affect both males and females and is present within all ethnicities. Keratoconus can be diagnosed through a routine eye exam. This condition generally involves both eyes, although one eye may be more affected than the other.
Symptoms
Keratoconus causes blurry or distorted vision as the result of a cone-shaped cornea. Symptoms can also include increased sensitivity to light and glare, eye redness or swelling. In later stages, keratoconus symptoms can include nearsightedness or astigmatism, and an inability to wear contact lenses due to the shape of the cornea.
Treatment
Keratoconus treatment depends on your symptoms. When your symptoms are mild, your vision can be corrected with eyeglasses. For moderate symptoms, you may need to wear special hard contact lenses to help keep your vision in proper focus.
Other ways that your ophthalmologist might treat moderate to advanced keratoconus:
Collagen Cross-Linking
Your ophthalmologist uses a special UV light and eye drops to strengthen the cornea. Doing this helps to flatten or stiffen your cornea, keeping the condition from progressing further.
Corneal Transplant
When symptoms are severe, your ophthalmologist may suggest a corneal transplant (DMEK). This is an out-patient surgical procedure that replaces all or part of your diseased cornea with healthy donor cornea tissue.
